The male reproductive system includes the scrotum, testes, seminal ducts, sex glands, and penis. These organs work together to produce sperm, male gametes, and other sperm components. These organs also work together to carry sperm out of the body and into the vagina, where it will help fertilize the egg to produce offspring ... [Read below]
[Top start] ... Scrotum
The scrotum is a burso-like organ made from the skin and muscles where the testes are located. It is located lower than the penis in the pubic region. The scrotum consists of 2 testicular sacs located side by side. The smooth muscles that make up the scrotum allow them to regulate the distance between the testes and the rest of the body. When the testicles become too warm to support spermatogenesis, the scrotum relaxes to move the testicles away from heat sources. Conversely, the scrotum moves with the testes closer to the body when the temperature falls below the ideal range for spermatogenesis.
Testes
The 2 testicles, also known as the testes, are the male sex glands responsible for the production of sperm and testosterone. Testes are ellipsoidal glandular organs about 4 to 5 cm long and 3 cm in diameter. Each testis sits inside its own sac on one side of the scrotum and is connected to the abdomen by a cord and cremaster muscle. Inside, the testes are divided into small compartments known as lobules. Each lobule contains a section of seminiferous tubules lined with epithelial cells. These epithelial cells contain many stem cells that divide and form sperm through the process of spermatogenesis.
Appendages
The epididymis is a storage area for sperm that wraps around the upper and posterior edges of the testes. The appendage consists of several long, thin tubes that are tightly coiled into a small mass. Sperm are produced in the testes and pass into the epididymis to mature before being passed through the male reproductive organs. The length of the epididymis delays the release of the sperm and gives them time to mature.
The spermatic cord and the vas deferens
In the scrotum, a pair of spermatic cord connects the testes to the abdomen. The spermatic cord contains the vas deferens along with the nerves, veins, arteries, and lymphatic vessels that support the function of the testes.
The vas deferens is a muscular tube that carries sperm from the epididymis into the abdomen into the ejaculatory canal. The vas deferens is wider in diameter than the epididymis and uses its internal space to store mature sperm. The smooth muscles of the walls of the vas deferens are used to move sperm to the ejaculatory duct through peristalsis.
Seminal vesicles
The seminal vesicles are a pair of lumpy exocrine glands that store and produce some of the liquid semen. The seminal vesicles are about 5 cm long and located behind the bladder closer to the rectum. The seminal vesicle fluid contains proteins and phlegm and has an alkaline pH to help sperm survive in the acidic environment of the vagina. The liquid also contains fructose to feed the sperm cells so that they survive long enough to fertilize the egg.
Seed ejection channel
The vas deferens passes through the prostate and joins the urethra in a structure known as the ejaculatory canal. The ejaculatory canal also contains channels from the seminal vesicles. During ejaculation, the ejaculatory canal opens and expels semen and secretions from the seminal vesicles into the urethra.
Urethra
Sperm travels from the ejaculatory canal to the outside of the body through the urethra, a 20 to 25 cm long muscular tube. The urethra runs through the prostate and ends at the outer opening of the urethra, located at the end of the penis. When urine leaves the body, from the bladder, it passes through the urethra.
The prostate gland, the size of a walnut, borders the lower end of the bladder and surrounds the urethra. The prostate produces most of the fluid, which is semen. This liquid is milky white and contains enzymes, proteins and other chemicals to support and protect sperm during ejaculation. The prostate also contains smooth muscle tissue that can contract to prevent the flow of urine or semen.
Cooper glands
Cooper's glands, also known as bulbourethral glands, are a pair of pea-shaped exocrine glands located below the prostate gland and up to the anus. Cooper's glands secrete a thin, alkaline fluid into the urethra, which lubricates the urethra and neutralizes acid from the urine that remains in the urethra after urination. This fluid enters the urethra during sexual arousal prior to ejaculation to prepare the urethra for semen flow.
Penis
The penis is the male external genital organ located above the scrotum and below the navel. The penis is roughly cylindrical in shape and contains the urethra and the external opening of the urethra. Large pockets of erectile tissue in the penis allow it to fill with blood and become erect. Excitation of the penis leads to its enlargement. The function of the penis is to deliver sperm to the vagina during intercourse. In addition to its reproductive function, the penis also allows urine to pass through the urethra to the outside of the body.
Sperm
Sperm is the fluid produced by males for sexual reproduction and ejaculated from the body during intercourse. Sperm contains sperm, the male sex gametes, along with a variety of chemicals suspended in a liquid medium. The chemical composition of semen gives it a thick, sticky consistency and a slightly alkaline pH. These traits help sperm support reproduction by helping sperm stay in the vagina after intercourse and to neutralize the acidic environment of the vagina. In healthy adult males, semen contains about 100 million sperm cells per milliliter. These sperm cells fertilize oocytes inside the female fallopian tubes.
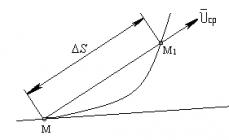
Spermatogenesis
Spermatogenesis is the process of sperm production that takes place in the testes and epididymis of adult males. Before puberty, there is no spermatogenesis due to the lack of hormonal triggers. During puberty, spermatogenesis begins when enough luteinizing hormone (LH) and follicle-stimulating hormone (FSH) are produced. LH triggers testosterone production by the testes, while FSH triggers the maturation of germ cells. Testosterone stimulates stem cells in the testes known as spermatogonia. Each diploid spermatocyte goes through the meiosis I process and is broken down into 2 haploid secondary spermatocytes. Secondary spermatocytes pass through meiosis II to form 4 haploid cell spermatids. Spermatids cells go through a process known as spermatogenesis, where they grow a flagellum and develop the structure of the sperm head. After spermatogenesis, the cell finally turns into spermatozoa. Spermatozoa are released into the epididymis, where they complete their maturation and become able to move on their own.
Fertilization
Fertilization is the process by which a sperm cell combines with an oocyte or egg cell to become a fertilized zygote. Sperm released during ejaculation must first swim through the vagina and uterus into the fallopian tubes, where they can find the egg. When faced with an egg, the sperm must penetrate the layers of the oocyte. Sperm contain enzymes in the acrosomal region of the head, which allows them to penetrate these layers. Once inside the oocyte, the nuclei of these cells fuse to form diploid cells known as the zygote. The zygote cell begins cell division to form an embryo.
In all world cultures, the function of reproduction, procreation, is considered one of the main ones. The male and female reproductive systems have different structures, but they perform one task: to form sex cells - gametes, when they merge at the moment of fertilization, the development of the future human body will become possible. This article is devoted to the study of the structure and function of the female reproductive system.
General characteristics of the reproductive organs of a woman
The female reproductive system includes the external and internal genital organs, which are also called reproductive (reproducing).
The outer ones, called the vulva, are visually pronounced to a sufficient degree - these are the pubis, labia majora and small labia, the clitoris and the entrance to the vagina (vagina), closed by an elastic hymen, called the virgin. Let's study the external organs of the female reproductive system in more detail.
Pubic structure
The lower abdomen at the level of the pubic (pubic bone) forms the pubis. The bone itself, at an anatomically correct position, hangs over the entrance to the vagina and looks like an arch. Externally, the pubis has a roller-like shape, forming an eminence. A layer of fat forms under his skin. Outside, a hairline is formed on it. It has a clearly defined horizontal border. If a woman's body produces an excessive amount of androgens - male sex hormones, the hairline increases and rises up at an acute angle to the navel. Pathology of pubic hair is a sign of sexual development.
Large and small labia
From the pubis to the anus, there are two folds of skin - the labia majora, which have an outer hairline and a layer contained in their connective tissue, the ducts of the Bartholin gland. It secretes fluid that moisturizes the female genitals. In case of violation of hygiene, harmful microorganisms penetrate into the tissues of the gland and cause inflammation in the form of painful seals.
Under the large lips are the labia minora, densely braided with blood vessels and nerves. In their upper part there is an organ homologous to the male penis - the clitoris. Its growth is inhibited by the hormones of the female reproductive system - estrogens. The clitoris contains a large number of nerves and blood vessels, which means it is highly sensitive. If the size of the clitoris is greatly increased in a girl or woman, this may be a clear sign of hormonal pathology.

Vaginal entrance
The vulva, in addition to the pubis, labia majora and small labia, the clitoris includes the entrance to the vagina. The hymen is located at a distance of up to 2 centimeters from it. It consists of connective tissue and has several holes through which blood flows during menstruation.
Internal reproductive organs of a woman
These include the vagina (vagina), uterus, ovaries, and fallopian tubes. All of them are located in the pelvic cavity. Their functions are in the maturation and entry of fertilized female gametes-eggs into the uterine cavity. In it, the embryo will develop from the zygote.
The structure of the vagina
The vagina is an elastic tube made up of muscle and connective tissue. It is located from the genital slit towards the uterus and has a length of 8 to 10 cm. Located in the small pelvis, the vagina enters the cervix. It has anterior and posterior walls, as well as a fornix - the upper part of the vagina. The posterior fornix of the vagina is deeper than the anterior.

The vagina is located at an angle of 90 degrees to the surface of the uterus itself. Thus, the internal female genital organs, which include the vagina, are densely entwined with arterial and venous vessels, as well as nerve fibers. The vagina is separated by a thin connective tissue wall from the bladder. It's called the vesicovaginal septum. The lower part of the vaginal wall is rearwardly separated from the lower part of the large intestine by the perineal body.
Neck and function
The vagina enters a canal called the cervical canal, and the junction itself is the external pharynx. Its shape differs in women who have given birth and who have not given birth: if the pharynx is point-oval, the uterus did not bear a fetus, and the type of gap is characteristic of those who have given birth. The uterus itself is an unpaired hollow muscular organ, consisting of a body and a neck and located in a small pelvis. Considering the structure of the female reproductive system and its functions, it becomes clear that she is responsible for the formation and development of the embryo, as well as for the process of pushing the fetus as a result of labor. Let's return to the structure of its lower section - the neck. It is connected to the top of the vagina and is shaped like a cone (in nulliparous women) or a cylinder. The vaginal portion of the cervix is up to three centimeters long and is also anatomically divided into the front and back lips. The cervix and pharynx transform with the woman's age.
Inside the cervix there is a cervical canal ending in an internal os. It is lined with mucus secreting secretory glands. If its secretion is disturbed, blockage and the formation of cysts can occur. The mucus has bactericidal properties and prevents infection of the uterine cavity. 4-6 days before the release of the egg from the ovary, the mucus becomes less concentrated, so sperm can easily penetrate through it into the uterus, and from there into the fallopian tubes.
After ovulation, the cervical secretion increases its concentration, and its pH decreases from neutral to acidic. The pregnant woman is covered with a clot of cervical mucus in the cervical region. During the menstrual period, the cervical canal opens slightly so that the torn layer of the endometrium can come out. This can be accompanied by aching pains in the lower abdomen. During labor, the cervical canal can open up to 10 cm in diameter. This contributes to the birth of a child.

Among the most common diseases of the cervix is its erosion. It appears as a consequence of damage to the mucous layer caused by infections or trauma (abortion, complicated childbirth). Timely undetected and untreated erosion can cause inflammation and even cancer.
Fallopian tubes
Fallopian tubes, also called oviducts or fallopian tubes, are 2 elastic tubes located in the abdominal cavity and entering the bottom of the uterus. The free edge of the oviduct has a fringe (fimbria). Their beating ensures the advancement of the egg that has emerged from the ovary into the lumen of the tube itself. The length of each oviduct is from 10 to 12 cm. It is divided into sections: a funnel, which has an expansion and is equipped with fimbria, an ampulla, an isthmus, a part of the canal entering the uterine wall. For the normal development of pregnancy, such a condition as complete patency of the oviducts is necessary, otherwise infertility awaits the woman. The most common pathologies of the fallopian tubes are adhesions, salpingitis and hydrosalpinx.
All of these diseases cause tubal infertility. They are complications of chlamydia, gonorrhea, trichomoniasis, genital herpes, causing narrowing of the lumen of the fallopian tubes. Frequent abortions can provoke the appearance of adhesions that are located across the tube. Hormonal disorders cause a decrease in the mobility of the ciliary epithelium lining the oviduct, which leads to a deterioration in the motor properties of the egg.

The most dangerous complication resulting from tubal pathologies is an ectopic pregnancy. In this case, the zygote stops in the oviduct without reaching the uterus. It begins to split and grow, stretching the tube wall, which eventually bursts. This results in severe, life-threatening internal bleeding.
Ovaries in women
They are a paired sex gland and weigh 6-8 grams. The ovaries are the production of sex hormones - estrogens, controlled by the pituitary gland and the hypothalamus - this is an intrasecretory function. Like the glands of external secretion, they form sex cells - gametes called oocytes. The biochemical composition and mechanism of action of estrogens will be studied by us later. Let's return to the structure of the female gonads - the ovaries. It should be borne in mind that the structure of the female reproductive system (as well as the male) is directly related to the urinary system.
It is from the mesonephros (primary kidney) that the stroma of the female gonads develops. The precursors of oocytes - oogonia, are formed from the mesenchyme. The ovary has a tunica albuginea, and under it there are two layers: cortical and cerebral. The first layer contains follicles, which, when mature, form oocytes of I and I order, and then mature eggs. The medulla of the gland consists of connective tissue and performs a supporting and trophic function. It is in the ovaries that ovogenesis occurs - the process of reproduction, growth and maturation of female reproductive gametes - eggs.
The specificity of a woman
The structure of the reproductive system of the female and male individuals is controlled by special biologically active substances - hormones. They are produced by the gonads: the testes in men and the ovaries in women. Entering the blood, they have a targeted effect on both the development of the reproductive organs and the formation of secondary sexual characteristics: body hair, the development of the mammary glands, the pitch and timbre of the voice. The development of the female reproductive system occurs under the influence of estradiol and its derivatives: estriol and estrone. They are produced by special ovarian cells called follicles. Female hormones - estrogens lead to an increase in the volume and size of the uterus, as well as to muscle contractions of the fallopian tubes and the uterus itself, that is, the genital organ is prepared for the adoption of the zygote.

The corpus luteum produces progesterone - a hormone that stimulates the development of the child's place - the placenta, as well as an increase in the glandular epithelium of the mammary glands during pregnancy. Violation of the hormonal background of the female body leads to diseases such as uterine fibroids, endometriosis, polycystic disease.
Anatomical features of the female uterus
The reproductive system of the female body has an organ that is unique in structure and function. It is located in the pelvic cavity between the bladder and rectum and has a cavity. This organ is called the uterus. To understand the mechanism of fertilization, remember that the genitals - the ovaries in women, are connected to the fallopian tubes. The egg, entering the oviduct, then enters the uterus, which serves as the organ responsible for the development of the embryo (embryogenesis). It consists of three parts: the neck, which was studied earlier, and the body and bottom. The body of the uterus looks like an inverted pear, into the expanded part of which two fallopian tubes enter.

The genital organ is covered with a connective tissue membrane and has two layers: muscular (myometrium) and mucous (endometrium). The latter is built from cells of squamous and columnar epithelium. The endometrium changes the thickness of its layer: during ovulation, it thickens, and if fertilization has not occurred - this layer is torn away along with a portion of blood from the walls of the uterus - menstruation occurs. During pregnancy, the volume and greatly increase (approximately 8-10 times). In the pelvic cavity, the uterus is suspended on three ligaments and braided with a dense network of nerves and blood vessels. Its main function is the development and nutrition of the embryo and fetus until the moment of physiological birth.
Pathology of the uterus
The structure of the female reproductive system may not always be ideal and correctly functioning. One of the pathologies of the reproductive system associated with the structure of the genital organ may be a two-horned uterus. It has two bodies, each of which is associated with one oviduct. If the pathology of the female reproductive system concerns the structure of the endometrium, they speak of hypoplasia and aplasia of the uterus. The consequence of all the above pathologies is the termination of pregnancy or infertility.
In this article, the anatomical and physiological features of the female reproductive system were studied.
The "aggregate" of the male genitals serves two purposes: the removal of urine from the body, and, most importantly, the creation and delivery of sperm... This is what determines the structure of the external genital organs, such as the penis and scrotum, which are responsible for the safety and comfortable conditions for the maturation of sperm in the testicles (rightly called the main organ in the male reproductive system).
Of course, for most men, what lies on the surface is much more interesting, namely, the external genital organs, because it is the penis that is a secret subject for pride or grief, rather than incomprehensible glands or testicles hidden from the eyes. What are these undoubtedly famous male organs?
Penis
Penis(penis or phallus - that's what the male external organ is called in medicine and literature) is an external organ of a man designed for sexual intercourse, the purpose of which is to eject semen and urine out of the bladder.
On average, according to anatomical statistics, the size of the external male genital organ (penis) in a calm state ranges from 4 to 8 centimeters, increasing with arousal by 2-4 times.
In the anatomy of the penis, a distinction should be made between:
- Root(base).
- Body(trunk), which is a sponge-like cavernous body with many internal voids designed to quickly fill with blood during preparation for intercourse.
- Head penis, covering the ends of the trunk and covered with delicate foreskin - the thinnest skin. In the central upper part of the head there is an opening, the so-called urethra, through which semen and urine are released. Also, the head, due to the huge number of nerve endings, is very sensitive to any touch, which plays an important role in the excitement of men.
 In an erect state, the penis expands by filling with blood. and acquires density and elasticity. Prolonged erection is possible due to the fact that the root of the penis consists of special, sufficiently powerful muscles that can block the flow of blood in a couple of seconds.
In an erect state, the penis expands by filling with blood. and acquires density and elasticity. Prolonged erection is possible due to the fact that the root of the penis consists of special, sufficiently powerful muscles that can block the flow of blood in a couple of seconds.
After the end of the act they relax gently, the member falls off and decreases in size... The head differs from the excited trunk by its softness and tenderness, which avoids injuries to the vagina, even with very active sex.
Speaking of injuries, it is purely many times more common than women, due to the fact that men put themselves more in danger. can lead to partial or complete removal of the male organ, or even to the death of a man, so you need to be careful.
During intercourse, two types of fluid are released:
- Smegma(a familiar lubricant) - the selection of the glands of the foreskin (the skin fold covering the head) to ensure a reduction in friction of the head and avoid the appearance of microtraumas. The grease is composed of fats and mycobacterial colonies. New discharge is white and plastic, but over time they turn yellow and acquire a pungent odor.
- Sperm(also known as seminal fluid) - consisting of two components: seminal plasma - a combined hodgepodge of the products of the activity of various glands and spermatozoa, the final product of the male reproductive system.
Scrotum
 Scrotum - musculocutaneous organ, designed to store the testes, epididymis and the beginning of the seminal canal. Each individual organ is enclosed in a kind of muscle capsule inside, which is especially clearly visible from the connecting seam that every man has.
Scrotum - musculocutaneous organ, designed to store the testes, epididymis and the beginning of the seminal canal. Each individual organ is enclosed in a kind of muscle capsule inside, which is especially clearly visible from the connecting seam that every man has.
The color of the skin on the scrotum is darker than the rest of the body, the skin is covered with hair, its density may vary.
The purpose of the scrotum is obvious - it creates optimal conditions for the maintenance of important internal reproductive organs. For example, to produce healthy sperm, the body temperature must be two degrees below the normal human body temperature.
It allows this to be achieved with the help of a unique system for maintaining the required temperature - this is how the scrotum is compressed in the cold, and when it is hot it moves away from the body as much as possible.
Abnormal development of the external genital organs in men
There are certain norms for the development of external genital organs. Deviation from these norms is abnormal..
Here are some examples of abnormal development of the penis:

- Congenital - the impossibility of full disclosure of the head due to accrete or insufficiently developed foreskin. The disease threatens the development of all kinds of infections and the complete impossibility of sexual intercourse, but it is usually diagnosed in the first years of a child's life and is successfully treated either by exercise or by surgery.
- Congenital absence of the penis or anomalies in the development of any of its parts, which include both the absence of the head and any violations of the integrity of the trunk (hidden in the body, for example, or bifurcated).
- Ectopia of the penis (another name, micropenis) is a developmental anomaly in which the penis grows up to one or two centimeters, and even in the active state does not increase by more than 3-4 centimeters, which naturally makes sex life completely impossible. Some men complain about the size of their genitals and in vain call theirs small, although, according to world medical standards, it has a normal, average size and does not require any increase.
- - an anomaly in the development of the urethra (the hole from which urine comes out and). The anomaly lies in the fact that the opening of the urethra can be located in an uncomfortable place for a man, for example, on the scrotum. Distinguish between different.
Mostly by surgeons as a measure, done so that in adulthood this disease does not interfere with a person.
More difficult to treat anomaly of the development of male genital organs than hypospadias. The essence of the diagnosis is that the opening of the urethra is not just in the wrong place, but it (the urethra) is simply split along.
Diseases of the genital organs in men
 The importance of all organs in the body is high, but the representatives of the stronger sex are most horrified when they notice any unpleasant ones. They are doing the right thing that they are terrified, I must say. And I must also say that it is necessary to take the most important measure - see a doctor.
The importance of all organs in the body is high, but the representatives of the stronger sex are most horrified when they notice any unpleasant ones. They are doing the right thing that they are terrified, I must say. And I must also say that it is necessary to take the most important measure - see a doctor.
A doctor who can do an examination and determine diseases, pathologies and anomalies of the male genital organs (inflammation, infectious, congenital, etc.) and in most cases can independently carry out treatment, taking into account the age characteristics of patients - an andrologist. He can define purely male, or diseases are common, but manifest differently than in women.
The figure clearly shows the structure of the system of male genital organs in the context:

Scroll down to read a description of what the internal genital organs of men are in physiology.

For the harmonious work of the male reproductive system, the participation of both external and internal genital organs is required. What do the internal genitals of men include?
Internal genital organs are subdivided into: testicles, vas deferens, prostate, spermatic cord and prostate.
It is worth considering in more detail the features and work of each of these bodies.
Testicles
Testicles(testicles) is a double gland responsible for the formation of sperm and the injection into the blood of the hormone testosterone, which is responsible for a man's sexual arousal. Testicle sizes on average range from four to six centimeters in length.
The testicles are located in the scrotum, where the testicles are separated by a special membrane (externally expressed by a suture on the scrotum). It is normal for the testes to be different in size or at different heights.
 Testicles, perhaps the most vulnerable organ of the male reproductive system.
Testicles, perhaps the most vulnerable organ of the male reproductive system.
So, for example, overheating is categorically contraindicated for them, because too high a temperature interferes with the development of sperm. The norm for good work of the testicles is a temperature not exceeding 32-33 degrees.
The scrotum is responsible for temperature control, but it may not cope with the task if, for example, a man is fond of hot baths, has a sedentary job, or wears overly tight underwear.
This lifestyle can lead to infertility and erection problems.
Seminiferous tubule
 The seminiferous tubule is organ designed to supply blood to the testicle and remove semen from it.
The seminiferous tubule is organ designed to supply blood to the testicle and remove semen from it.
A pair of convoluted seminiferous tubules extend from the epididymis with a total length of no more than 9 centimeters, whose interior is lined with epithelium in several layers.
They are surrounded by connective, rather loose tissue, permeated with many blood vessels. The sinuous canaliculi are connected in straight lines forming a single testicular network. The result of such a fusion is a dozen efferent tubules flowing into the duct of the epididymis.
The vas deferens
Seed deferens- these are special ducts into which the seminal fluid enters from the duct of the epididymis.
These are two organs, each about half a meter long, designed to eject semen. Starting from the epididymis, they pass through the inguinal canals and join into a common ejaculatory stream, which, after passing through the prostate gland, ends at the back of the urethra.

The rapid movement of seminal fluid along the stream is possible due to the contraction that occurs on the eve of orgasm.
At the peak of contractions, sperm enters the urethra, which is the moment of ejaculation.
Prostate
The prostate gland (prostate) is single organ through which the urethra passes, which is responsible for the production of secretions, which are an important component of semen.
Externally, the prostate gland resembles a capsule of dense elastic tissue, inside, it is filled with glandular tissue, whose glands produce a secret that is excreted into the prostate part of the urethra with the help of the contraction of the smooth muscles of the gland during ejaculation.
 The secret outwardly looks like an opaque white liquid. designed to dilute spermatozoa and ensure their rapid movement through the ducts.
The secret outwardly looks like an opaque white liquid. designed to dilute spermatozoa and ensure their rapid movement through the ducts.
Also, an increase in the total amount of seminal fluid provides a rich and vivid orgasm.
The prostate is completely formed by the time of the completion of puberty in men, further its growth and development stops.
Yet one small but important organ is the seminal vesicles - paired glands, responsible for the production of a secret consisting of protein and fructose. This semen supplement is necessary to energize the sperm and increase their chance of reaching a female egg.
Abnormal development and diseases of the internal genital organs in men
 If the abnormal development of the external genital organs leads to the impossibility of sexual intercourse, then any changes in the inner part of the male reproductive apparatus lead to the production of non-viable sperm, and, accordingly, to infertility.
If the abnormal development of the external genital organs leads to the impossibility of sexual intercourse, then any changes in the inner part of the male reproductive apparatus lead to the production of non-viable sperm, and, accordingly, to infertility.
The reasons for the malfunction of the internal genital organs can be different:
- Congenital or acquired as a result of surgery, the absence of one or two testicles.
- Adult-onset illnesses with sudden and prolonged fever, such as influenza, mumps, or measles.
- Pseudohermaphroditicity, expressed in the presence of a part of the female genital organs and atrophy of the testicles and prostate, which makes it impossible for both full sexual intercourse and the possibility of conception.
- - a disease in which one or two testicles did not descend into the scrotum, but remained in the abdominal cavity or groin.
- Groin injuries resulting in testicular malfunction or rupture of the seminal duct.
- Inflammatory processes caused by sexually transmitted diseases.
- The consequences of inflammation caused by the last stages of hemorrhoids, prostate cancer or urethra.
Only the joint work of both external and internal male genital organs will ensure the possibility of high-quality functioning of the entire genital apparatus.
Violations in the work of at least one of the organs caused by illness or negligence towards your body can lead to infertility or the complete impossibility of sexual intercourse.
A short video on the device (structure) of the internal and external male genital organs: find out what functions they perform and how the reproductive system works
All living things reproduce. Reproduction - the process by which organisms create more organisms like them - is one of the things that distinguishes living things from non-living things.
In humans, the male and female reproductive systems work together to make a baby. In the human reproductive process, two types of germ cells or gametes are involved.
The male gamete, or sperm, and the female gamete, egg or ovum, meet in a woman's reproductive system to create a child. The male and female reproductive systems are essential for reproduction.
People pass on some characteristics of themselves to the next generation through their genes, special carriers of human traits.
Parents of genes pass on to their offspring what makes children like others in theirs, but they also make each child unique. These genes come from the sperm of the father and the eggs of the mother, which are produced by the male and female reproductive systems.
Understanding the male reproductive system, what it does, and the problems that may affect it can help you better understand your child's reproductive health.
About the male reproductive system
Most species have two sexes: male and female. Each sex has its own unique reproductive system. They differ in shape and structure, but both are specifically designed to produce, feed, and transport either egg or sperm.
Unlike the female, whose genitals are located entirely inside the pelvis, the male has reproductive organs, or genitals, that are located inside and outside the pelvis. Male genitals include:
- testicles;
- the duct system, which consists of the epididymis and the vas deferens;
- accessory glands, which include the seminal vesicles and the prostate gland;
- penis.
In a guy who has reached puberty, two testicles (or testicles) produce and store millions of tiny sperm cells. The testicles are oval in shape and are about 2 inches (5 centimeters) long and 1 inch (3 centimeters) in diameter.
The testes are also part of the endocrine system as they produce hormones, including testosterone. Testosterone is a major part of puberty in boys, and as a guy makes his way through puberty, his testicles produce more and more.
Testosterone is a hormone that causes boys to produce deeper voices, larger muscles, body and facial hair, and stimulates sperm production.
Along with the testes are the epididymis and the vas deferens, which make up the duct system of the male reproductive organs.
Seed leakage is a muscle tube that runs up the testicles and transports a sperm fluid called sperm. Epididymis is a set of coiled tubes (one for each testicle) that connects to the seed of the seed.
The epididymis and testicles hang in a sac-like shape behind a pelvis called the scrotum. This bag of skin helps regulate the temperature of the testicles, which must be cooler than body temperature in order to produce sperm.
The scrotum changes size to maintain the correct temperature. When the body is cold, the scrotum contracts and stiffens to retain body heat.
When it heats up, the scrotum becomes larger and more flexible to get rid of the extra heat. This happens without the guy thinking about it. The brain and nervous system give the scrotum a cue to change its size.
Accessory glands, including the seminal vesicles and the prostate gland, provide fluids that lubricate the canal system and nourish sperm. The seminal vesicles are saccular structures attached to the vas deferens towards the bladder.
The prostate gland, which produces some parts of the sperm, surrounds the ejaculatory ducts at the base of the urethra, just below the bladder.
The urethra is the channel that carries sperm to the outside of the body through the penis. The urethra is also part of the urinary system because it is also the channel through which urine passes as it leaves the bladder and exits the body.
The penis actually has two parts: the shaft and the glans. The shaft is the main part of the penis, and the glans is the tip (sometimes called the glans).
At the end of the head, there is a small slit or hole in which seeds and urine exit the body through the urethra. The inside of the penis is made of spongy tissue that can expand and contract.
All boys are born with a foreskin, a fold of skin at the end of the penis that covers the glans. Some boys are circumcised, which means that the foreskin is cut off by a doctor or priest.
Circumcision is usually done during the first few days of a boy's life. Although circumcision is not a medical necessity, parents who choose to circumcise their sons often do so based on religious beliefs, hygiene concerns, or cultural or social reasons.
Boys who have their penises circumcised and those who do not are no different: all penises work and feel the same, regardless of whether the foreskin has been removed.
What does the male reproductive system do
The male reproductive organs work together to produce and release sperm into the female's reproductive system during intercourse. The male reproductive system also produces sex hormones that help a boy develop into a sexually mature person during puberty.
When a boy is born, he has all the parts of his reproductive system in place, but until puberty cannot reproduce. When puberty begins, usually between the ages of 9 and 15, the pituitary gland - which is located near the brain - secretes hormones that stimulate the testes to produce testosterone.
Testosterone production leads to a variety of physical changes. Although the timing of these changes is different for each guy, the stages of puberty usually follow a set sequence:
- During the first stage of male puberty, the scrotum and testes grow.
- Then the penis gets longer and the seminal vesicles and prostate gland grow.
- Hair begins to grow in the pubic area and then on the face and armpits. At this time, the boy's voice also increases.
- Boys also have a growth spurt during puberty as they reach their adult height and weight.
Sperm
Puberty males produce millions of sperm cells every day. Each sperm is extremely small: only 1/600 inch (0.05 millimeter). Sperm develops in the testes in a system of tiny tubes called seminiferous tubules.
At birth, these tubules contain simple round cells, but during puberty, testosterone and other hormones cause these cells to transform into sperm.
Cells divide and change until they have a head and short tail, like tadpoles. The head contains genetic material (genes).
The sperm use their tails to propel themselves towards the epididymis, where they complete their development. It takes about 4-6 weeks for sperm to pass through the epididymis.
The sperm then travels to the vas deferens or sperm. The seminal vesicles and the prostate gland form a whitish fluid called semen, which mixes with semen to form sperm when a man is sexually stimulated.
The penis, which usually hangs, becomes heavy when a man is sexually aroused. The tissues in the penis become filled with blood and become stiff and erect (erection). The stiffness of the penis makes it easier to insert into a woman's vagina during intercourse.
When the penis is stimulated, the muscles around the reproductive organs contract and force sperm to pass through the duct system and urethra. The semen is pushed out of the man's body through the urethra in a process called ejaculation. Every time a guy ejaculates, he can contain up to 500 million sperm.
When a female ejaculates during intercourse, the sperm is deposited in the female's vagina. From the vagina, sperm travels through the cervix and travels through the uterus using uterine contractions.
If a mature egg is in one of a woman's fallopian tubes, sperm alone can penetrate, as well as fertilization or conception. This fertilized egg is now called a zygote and contains 46 chromosomes - half of the egg and half of the sperm.
Genetic material from a man and a woman is combined so that a new person can be created. The zygote divides over and over again as it grows in the female uterus, maturing during pregnancy into an embryo, fetus, and finally a newborn baby.
 Sometimes boys have problems with the reproductive system, including:
Sometimes boys have problems with the reproductive system, including:
Traumatological trauma
Even mild injury to the testicles can cause severe pain, bruising, or swelling. Most testicular injuries occur when the testicles are bumped or crushed, usually during sports or other injury.
Testicle torsion when one of the testicles curls around, cutting off its blood supply, is also a medical emergency that is fortunately not common. Surgery is needed to unwind the cord and save the testicle.
Varicocele
This is a varicose vein (abnormally swollen vein) in the network of veins that run from the testicles. Varicoceles often develop while the boy is going through puberty.
Varicocele is usually not harmful, but can damage the testicle or decrease sperm production. Take your son to see his doctor if he is concerned about changes in his testicles.
Testicular cancer
It is one of the most common cancers in men under 40. It happens when cells in the testicle divide abnormally and form a tumor.
Testicular cancer can spread to other parts of the body, but if detected early, the rate of healing is excellent. Adolescent boys should be encouraged to learn how to do testicular self-tests.
Epididymitis
It is inflammation of the epididymis, the spiral tubes that connect the testes to the testes. It is usually caused by an infection such as sexually transmitted chlamydia and results in pain and swelling near one of the testicles.
Dropsy
A hydrocele is when fluid collects in the membranes that surround the testes. Hydrocellae can cause swelling in the scrotum around the testicle, but is usually painless. In some cases, surgery may be required to correct the condition.
Inguinal hernia
When part of the intestine enters through an abnormal opening or weakening of the abdominal wall and into the groin or scrotum, it is known as an inguinal hernia. A hernia may look like a bulge or swelling in the groin area. It is treated with surgery.
Disorders affecting the penis include:
- Inflammation of the penis. Symptoms of penile inflammation include redness, itching, swelling, and pain. Balanitis is when the glans (the head of the penis) become inflamed. Post-hit is an inflammation of the foreskin, usually due to yeast or a bacterial infection.
- Hypospadias. In this disorder, the urethra opens on the underside of the penis rather than at the tip.
- Phimosis. This is the tightness of the foreskin of the penis and is common in newborns and young boys. It usually gets better without treatment. If it interferes with urination, circumcision (removal of the foreskin) may be recommended.
- Paraphimosis. It can develop when the foreskin of a boy's uncircumcised penis is abducted (pulled away to expose the head) and trapped so that it cannot be returned to an unprofitable position. As a result, blood flow to the head of the penis may be affected and the boy may have pain and swelling. The doctor may use lubricant to make a small incision so that the foreskin can be pulled forward. If that doesn't work, circumcision is recommended.
- Ambiguous genitals. For most boys born with this disorder, the penis may be very small or nonexistent, but testicular tissue is present. In a small number of cases, a child may have both testicles and ovarian tissue.
- Micropenis. It is a disorder in which the penis, although usually formed, is well below the average size as defined by standard measurements.
If your son has symptoms, problems with his reproductive system, talk to your doctor - many problems with the male reproductive system can be treated. The doctor is also a good resource for your son if he has questions about growth and sexual development.